HIPEC & Cytoreductive Surgery in Nagpur (Peritoneal Cancer Treatment)
A comprehensive, patient-friendly guide to Cytoreductive Surgery (CRS) and
HIPEC (heated chemotherapy delivered inside the abdomen) for selected cases of
peritoneal cancer.
If you or a family member has been told “cancer has spread in the abdomen / peritoneum,” this page explains what CRS + HIPEC means, when it may be considered, how evaluation usually works, and what recovery can look like.
What you’ll find on this page
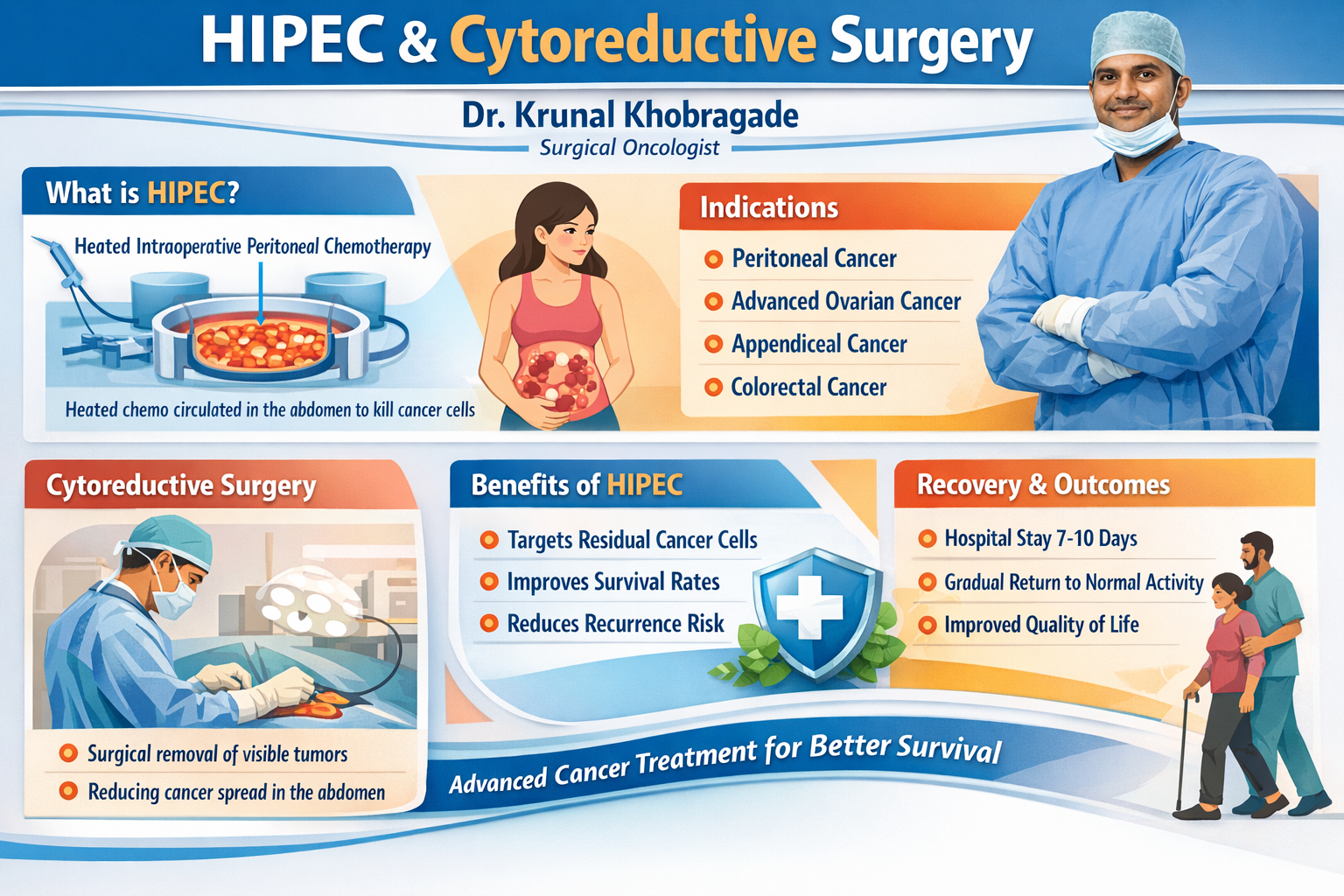
What is HIPEC?
HIPEC stands for Hyperthermic Intraperitoneal Chemotherapy. In simple words, it is chemotherapy delivered directly inside the abdomen during surgery, after visible tumor deposits have been removed as much as possible.
- “Intraperitoneal” means the medicine is circulated within the abdominal cavity (the peritoneal space).
- “Hyperthermic” means the solution is warmed. Heat can help chemotherapy work locally in some situations.
- Local delivery aims to expose the peritoneal surfaces to the drug where disease can spread in thin layers.
HIPEC is not a standalone “one-step” treatment. It is typically considered as part of a combined approach with cytoreductive surgery (CRS) in carefully selected cases.
What is Cytoreductive Surgery (CRS)?
Cytoreductive surgery (often called “CRS”) is a surgery aimed at removing visible cancer deposits from the peritoneal surfaces and involved areas inside the abdomen.
The intent is to reduce tumor burden as much as safely possible. The exact steps vary from patient to patient, depending on where deposits are located and the overall health condition.
Why CRS is discussed along with HIPEC
- Peritoneal disease can appear as multiple small deposits on peritoneal surfaces.
- CRS focuses on removing visible disease; HIPEC is discussed as a method of local chemotherapy exposure afterward.
- Whether CRS + HIPEC is appropriate depends on many factors (disease extent, organ involvement, overall fitness, and more).
Who may be considered for CRS + HIPEC?
CRS + HIPEC is usually discussed for selected patients with peritoneal involvement where the disease is primarily within the abdominal cavity and where a multidisciplinary team believes a combined approach may be reasonable.
Common clinical scenarios where CRS + HIPEC may be discussed
- Peritoneal cancer / peritoneal metastasis from certain primary cancers (for example: colorectal, appendix, ovarian, stomach in selected situations).
- Pseudomyxoma peritonei (mucinous disease in the peritoneum) in appropriate candidates.
- Selected cases where imaging and clinical evaluation suggest the disease burden may be surgically addressable.
Not everyone with “peritoneal spread” is a candidate for CRS + HIPEC. The decision depends on extent of disease, organ involvement, overall fitness, and the expected balance of risks and potential benefit in that individual situation.
How evaluation & decision-making typically happens
Before planning CRS + HIPEC, doctors usually do a structured assessment to understand: where the disease is, how extensive it is, and how safe surgery may be.
Typical steps in evaluation
- Detailed history & examination: symptoms, prior treatments, overall stamina, medical conditions.
- Imaging review: CT/MRI/PET-CT (as appropriate) to understand distribution and organ involvement.
- Blood tests: to assess organ function, nutrition, anemia, and baseline parameters.
- Review of pathology: biopsy/surgery reports to confirm cancer type and behavior.
- Multidisciplinary discussion: surgical oncology, medical oncology, radiology, anesthesia, and supportive care inputs.
Questions commonly clarified during evaluation
- Is the disease mainly within the peritoneal cavity, or is there extensive spread elsewhere?
- Is it technically feasible to remove visible deposits safely?
- Is the patient medically fit for a long, complex abdominal surgery and recovery?
- What is the role of systemic chemotherapy before or after surgery (if advised)?
What happens on the day of CRS + HIPEC?
Every patient’s surgical plan is different. The broad workflow usually looks like this:
- Anesthesia & surgical access: the surgery begins under general anesthesia.
- Cytoreduction: removal of visible tumor deposits where feasible and safe (may involve peritoneal surfaces and selected organ/segment resections as needed).
- HIPEC phase: warmed chemotherapy solution is circulated in the abdomen for a defined period (protocol varies by situation).
- Completion & closure: reconstruction/closures and post-op stabilization.
- ICU/HDU monitoring: many patients need close monitoring immediately after surgery.
The exact duration, extent of organ work, and post-operative stay vary widely. Your treating team will explain the plan based on your diagnosis, imaging, prior treatment, and overall condition.
Risks, side-effects, and common concerns
CRS + HIPEC is a complex procedure and can carry significant risks. Discussing risks clearly is an important part of planning. The list below is not exhaustive and varies by individual case.
Possible risks after major abdominal surgery
- Bleeding, infection, wound complications
- Blood clots (DVT/PE) and breathing complications
- Delayed bowel movement (ileus), nausea, temporary feeding difficulties
- Fluid shifts, electrolyte imbalance, need for close monitoring
Procedure-specific considerations (varies by protocol and patient)
- Stress on kidneys/liver depending on the chemotherapy agent and patient condition
- Bone marrow suppression risk (in some situations)
- Risk of leaks or fistula when bowel resections are involved
- Longer hospitalization and recovery timeline compared to simpler surgeries
Recovery, follow-up, and return to routine
Recovery is individual. Many patients need a structured plan for nutrition, mobilization, wound care, and follow-up visits.
What recovery often includes
- Early mobilization: gradual movement with support to reduce complications.
- Nutrition plan: stepwise diet progression depending on bowel recovery and tolerance.
- Pain control: tailored to enable breathing exercises and movement.
- Monitoring: labs, imaging (if needed), and clinical checks based on progress.
- Oncology coordination: discussion on further systemic therapy or surveillance as advised.
Ask your treating team about “red flag symptoms” after discharge (fever, increasing abdominal pain, persistent vomiting, breathing trouble, wound issues, reduced urine output, or unusual swelling).
Consultation for HIPEC & Peritoneal Cancer Care (Nagpur)
If you have reports such as CT/MRI/PET-CT, biopsy/pathology, discharge summaries, or chemotherapy details, bring them along. A structured review helps clarify diagnosis, stage, and suitable next steps.
This page is for educational understanding and does not replace a medical consultation. Treatment decisions are individualized.
FAQs: HIPEC & Cytoreductive Surgery
Systemic chemotherapy is delivered into the bloodstream (IV) and circulates throughout the body. HIPEC is delivered inside the abdomen during surgery to expose peritoneal surfaces locally. The two approaches are different, and in some situations both may be part of a broader plan.
The decision is based on multiple factors: the cancer type, disease distribution in the abdomen, whether there is major disease outside the abdomen, overall medical fitness, and feasibility of safe cytoreduction. Your reports, imaging, and treatment history guide the recommendation.
Not necessarily. Peritoneal disease can vary widely in extent and biology. Some patients may be managed with systemic therapy, some may be considered for surgery-based strategies, and some may need supportive/palliative approaches. The plan is individualized.
- Latest imaging (CT/MRI/PET-CT) with reports and CDs/links
- Biopsy/pathology report
- Discharge summaries (if any surgery was done)
- Details of chemotherapy (cycles, drugs, dates) and response assessments
- Current medications and any other medical conditions
Recovery timelines vary depending on the extent of surgery, resections performed, overall health, and post-op course. Your team will guide you on expected hospital stay, nutrition progression, activity levels, and follow-up schedule.
