Whipple’s Surgery (Pancreaticoduodenectomy) in Nagpur
A patient-first guide designed for families researching Whipple’s surgery—what it involves, how the decision is made, what to prepare, and what questions to ask during consultation.
Important: This page is for general education and does not replace medical advice. Treatment decisions depend on individual evaluation.
What is Whipple’s Surgery?
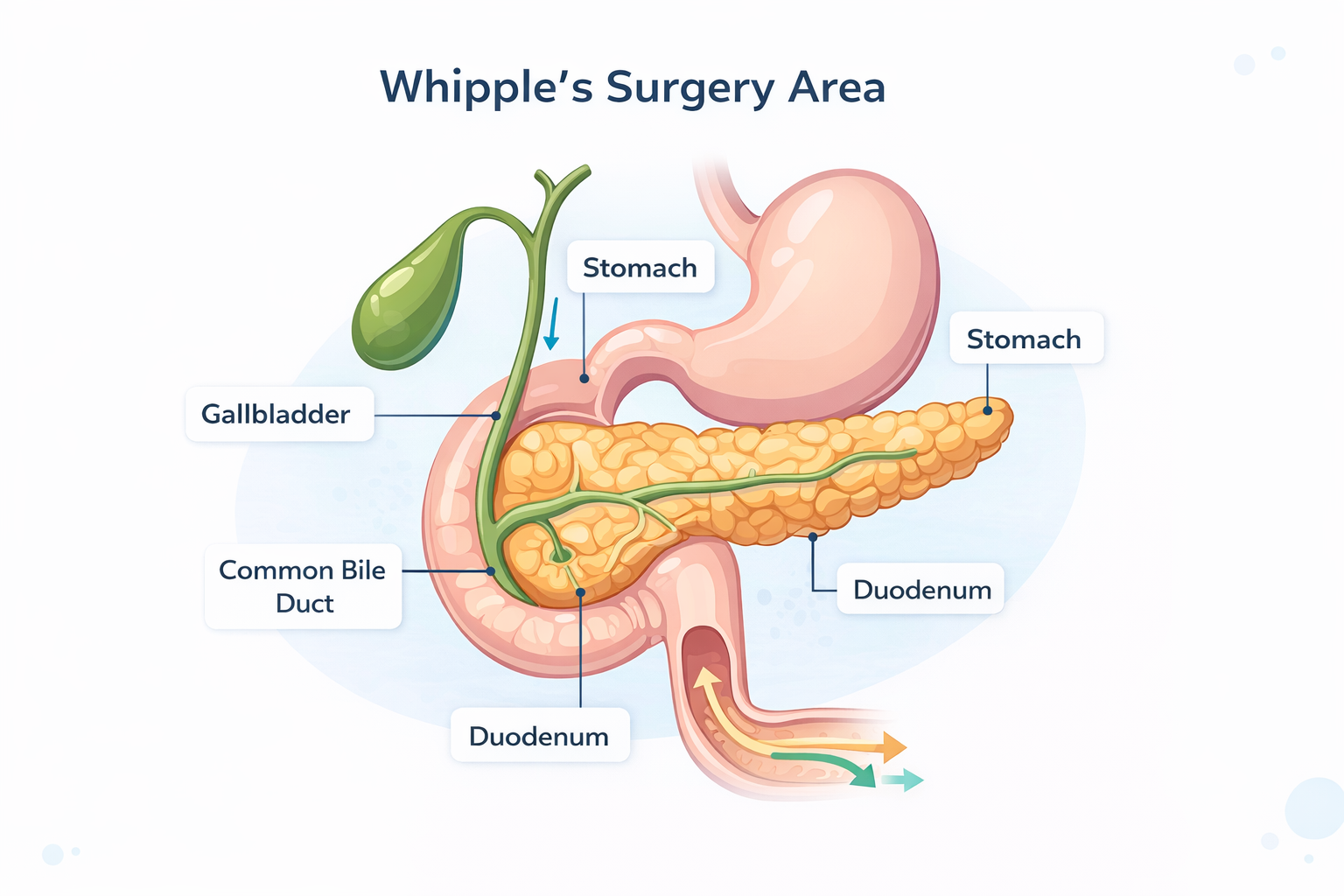
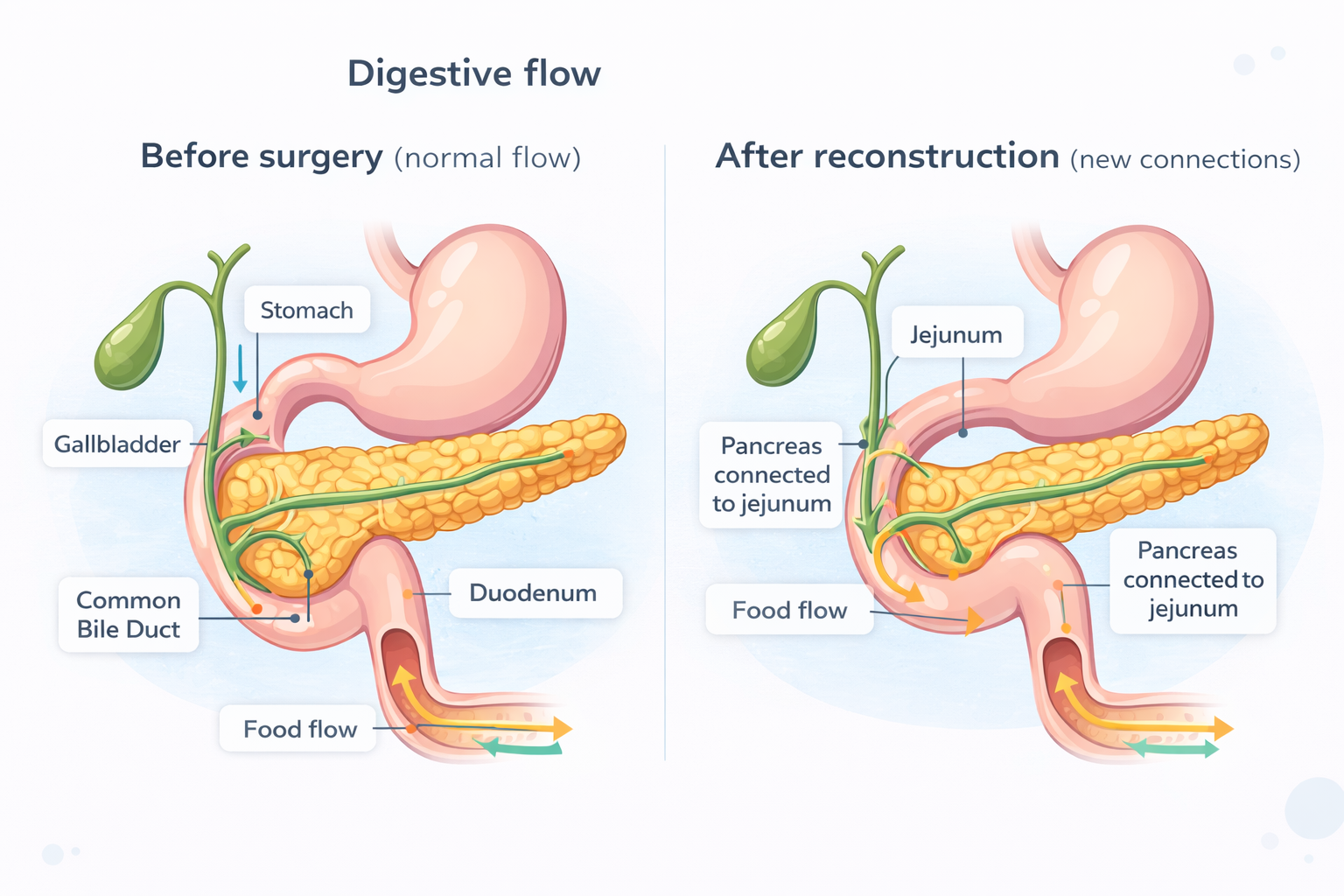
Whipple’s surgery, also called pancreaticoduodenectomy, is a complex operation performed for select conditions involving the head of the pancreas, duodenum, bile duct, and sometimes the stomach. The operation involves removing affected parts and then carefully reconstructing the digestive pathway so that food and digestive juices can flow again.
Simple mental model (without medical jargon)
- Remove the diseased part (where the problem is located).
- Reconnect the remaining pancreas, bile duct, and stomach/intestine back to the intestine.
- Restore flow of food, bile, and pancreatic enzymes in a controlled way.
There are multiple variations (for example, classic Whipple vs pylorus-preserving). Which approach is suitable depends on the patient’s anatomy, diagnosis, and the extent/location of disease seen on imaging.
Who may need Whipple’s Surgery?
Whipple’s surgery may be considered when a condition is located in the pancreatic head/nearby region and is suitable for surgical removal based on evaluation. Common situations where it may be discussed include:
Cancer-related indications
- Suspected or confirmed tumors of the pancreatic head
- Tumors of the ampulla (where bile duct meets intestine)
- Cancers of the distal bile duct
- Select duodenal tumors near the pancreas
Non-cancer indications (select cases)
- Certain complex benign tumors or pre-cancerous lesions
- Complicated chronic pancreatitis affecting the head region (case-dependent)
- Structural/obstructive conditions where reconstruction is needed (rare)
Not everyone with a pancreatic/bile duct condition requires Whipple’s surgery. The decision is individualized after imaging, staging, and clinical assessment.
When Whipple’s Surgery may not be advised
Whipple’s surgery is only recommended when the expected benefits of surgical removal outweigh the risks. It may not be advised in scenarios such as:
- When imaging suggests disease spread where surgery is unlikely to help (based on staging and oncology evaluation)
- When tumor involvement with major vessels is extensive and not surgically manageable (case-dependent)
- When overall health status makes major surgery unsafe without optimization
- When alternate treatment pathways are more appropriate after multidisciplinary review
What matters most
The decision is not only about “can surgery be done?” but also “is it the right next step for this specific patient now?” That’s why staging, nutrition, fitness, and comorbidity review are important.
How doctors decide if Whipple’s Surgery is suitable
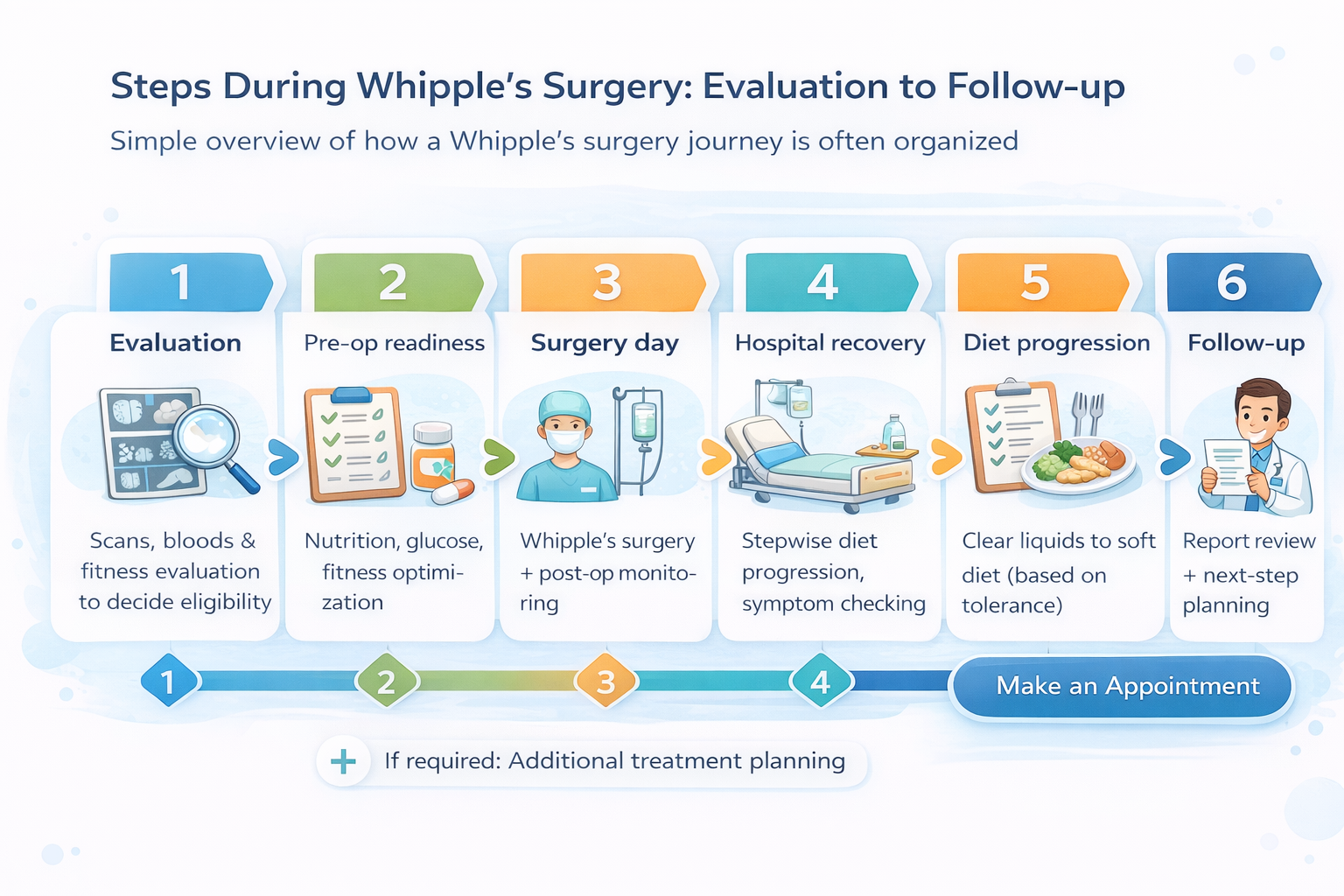
The evaluation typically focuses on three areas: (1) diagnosis & staging, (2) operability, and (3) fitness for surgery. Your consultation may include discussion around:
Reports & symptoms
Symptoms like jaundice, weight loss, upper abdominal pain, appetite changes, itching, pale stools, or dark urine may guide further testing, but diagnosis relies on imaging and lab findings.
Imaging (the “map”)
CT / MRI / MRCP / PET-CT (as advised) help understand location, size, relation to vessels, and any signs of spread. These scans inform whether the condition is potentially resectable.
Tissue diagnosis (when needed)
EUS-guided biopsy or other methods may be suggested in some cases. In other cases, decision-making may rely on imaging and clinical judgement. Your doctor will explain why and when biopsy is important.
Pre-operative readiness
Nutrition, diabetes status, liver function, heart/lung evaluation, anemia, and infection risk are reviewed. Some patients benefit from “prehabilitation”—a short period of strengthening and nutrition optimization before surgery, if clinically appropriate.
What to bring for consultation (practical checklist)
- All scan CDs/links + reports (CT/MRI/PET if done)
- Recent blood reports (LFT, CBC, sugars, tumor markers if available)
- Any endoscopy/EUS/biopsy reports
- Discharge summaries (if admitted previously)
- List of medicines + known allergies
- History of diabetes, BP, heart/lung conditions
What happens during Whipple’s Surgery (step-by-step, patient-friendly)
While surgical details vary per case, the procedure generally involves two major phases: resection (removal) and reconstruction (reconnection).
Phase A: Removal (Resection)
- Removal of the head of pancreas
- Removal of duodenum (first part of small intestine)
- Removal of gallbladder and part of bile duct (often)
- Sometimes a portion of stomach (depending on technique)
- Regional lymph node assessment/removal (as per oncology principles)
Phase B: Reconnection (Reconstruction)
- Connecting pancreas to intestine (for enzyme flow)
- Connecting bile duct to intestine (for bile flow)
- Connecting stomach to intestine (for food passage)
Why reconstruction is a big part of recovery
After surgery, digestion may take time to adjust because the pathway of food and digestive juices has been rerouted. Your care team typically guides diet progression, symptom monitoring, and medication support based on individual needs.
If you are researching robotic approaches, the decision on approach (open / laparoscopic / robotic) is individualized and depends on diagnosis, anatomy, surgeon assessment, and overall treatment plan.
Hospital stay, recovery and follow-up: what to expect
Recovery varies between individuals. Most patients go through a structured pathway: early mobilization, stepwise diet progression, pain control, monitoring of vitals and labs, and wound/drain care when applicable.
Early phase
First days
Focus on pain control, breathing exercises, walking, and monitoring.
Diet phase
Stepwise
Clear liquids → soft diet → individualized plan as tolerated.
Follow-up
Structured
Report review, pathology discussion (if applicable), next-step planning.
Common recovery topics families ask about
- Energy & fatigue: gradual improvement with nutrition and activity progression
- Weight & appetite: diet planning may be needed; small frequent meals are often discussed
- Blood sugar: pancreas-related surgery may affect glucose control; monitoring is important
- Digestion: enzyme support may be considered in some patients (doctor decides)
- Pathology report: helps guide next-step treatment planning where applicable
Caregiver notes (practical)
- Maintain a single folder for reports, discharge summary, prescriptions, follow-up dates
- Track symptoms daily (pain, fever, appetite, bowel changes) and share during follow-up
- Ask for a clear “diet progression” plan before discharge
- Confirm how to reach the clinic for post-discharge queries
Food, digestion and lifestyle after Whipple’s Surgery
Many families search online for “what can we eat after Whipple’s surgery?” The practical answer is: diet is progressed in stages, and recommendations are individualized based on tolerance, nutritional status, and symptoms.
Food strategy that is commonly discussed
- Smaller, frequent meals instead of heavy portions
- Protein-focused intake (as advised)
- Hydration planning
- Monitoring for intolerance to oily/spicy foods (case-dependent)
What to avoid doing on your own
- Self-prescribing supplements without discussing interactions
- Drastic fasting/“detox” diets during recovery
- Changing diabetes medicines without guidance
- Using random online diet charts without personalization
Your doctor may coordinate diet support or recommend a nutrition plan if needed, especially when appetite/weight loss is significant.
Questions to ask during consultation (high-signal, not generic)
If you are preparing for your visit, these questions can help you understand the plan clearly. You can screenshot this section.
About diagnosis & next steps
- What is the working diagnosis based on current scans?
- Is any additional imaging or biopsy needed before deciding?
- How do we determine staging and operability in my case?
About surgery planning
- Which Whipple technique is being considered and why?
- What is the plan for reconstruction and recovery monitoring?
- What are the “red flags” after discharge that need urgent attention?
About long-term care
- How will the pathology report be explained and used for next steps?
- Will I need additional therapy after surgery (if applicable)?
- What follow-up schedule should we plan for?
Book a consultation for Whipple’s Surgery evaluation in Nagpur
If you have scan reports, lab reports, or biopsy details, keep them ready. The consultation focuses on understanding your case and outlining possible next steps.
We avoid making guarantees online. The right plan is decided after reviewing your reports and clinical evaluation.
Quick preparation
- Bring CT/MRI/PET reports & CDs
- Blood tests (LFT/CBC/Sugars)
- Biopsy/EUS reports (if done)
- Medication list + allergies
Tip: Put everything in a single PDF folder for easier review.
FAQs about Whipple’s Surgery
Not always. It may be discussed for conditions in and around the pancreatic head region, including select bile duct, ampullary, and duodenal tumors. The exact indication depends on diagnosis and evaluation.
Operability is assessed using imaging (CT/MRI/MRCP/PET-CT as advised), clinical findings, and sometimes biopsy. Key considerations include location, relationship to vessels, and evidence of spread.
Not in every case. Some scenarios require tissue confirmation, while others rely on imaging and overall clinical judgement. Your doctor will explain what is appropriate in your situation and why.
Typically: scan CDs/links with reports, blood tests (LFT/CBC/sugars), any endoscopy/EUS/biopsy reports, discharge summaries (if any), medication list, and details of existing health conditions.
Digestion can take time to adjust because the pathway is reconstructed. Diet is usually progressed step-by-step, and some patients may need additional support depending on symptoms and nutritional status.
Since the pancreas plays a role in glucose regulation, blood sugar monitoring is often discussed—especially in patients with diabetes or borderline sugars. Management is individualized by the treating team.
Recovery timelines vary. Most patients return to activities gradually with a structured follow-up plan. Your doctor will guide you based on your recovery and condition.
Keep reports organized, follow diet progression instructions, monitor symptoms (fever, worsening pain, vomiting, jaundice, new swelling), and keep follow-up dates fixed. Ask the clinic how to reach the team for post-discharge questions.
If you want a broader view of digestive cancers and advanced oncology options, explore the related pages below.
