Robotic & GI Cancer Surgery in Nagpur
This hub page explains how robotic and minimally invasive approaches may be used in gastrointestinal (GI) cancer surgeries—covering pancreas, stomach, colorectal, liver, gallbladder, and complex abdominal cancers. It also helps you navigate related procedure pages, FAQs, and next steps for consultation.
What you’ll find on this page:
A clear overview of robotic GI cancer surgery, when it may be considered, the typical care pathway,
preparation and recovery guidance, and internal links to dedicated pages like
Whipple’s Surgery in Nagpur.
Note: Treatment decisions depend on diagnosis, stage, overall health, and surgical assessment. This page is informational and not a substitute for medical advice.
Looking specifically for pancreatic surgery? Start here: Whipple’s Surgery (Pancreaticoduodenectomy).
What is Robotic GI Cancer Surgery?
Robotic surgery is a type of minimally invasive surgery where the surgeon operates using advanced instruments and a high-definition 3D view. In GI cancer surgery, it may be used for selected cases involving organs such as the pancreas, stomach, colon/rectum, liver, and gallbladder. The choice of approach (open, laparoscopic, or robotic) depends on the cancer type, stage, anatomy, prior surgeries, and the complexity of the operation.
How it differs from open surgery
- Smaller incisions in many cases
- Camera-based visualization
- Instrument precision in tight spaces (case-dependent)
- Approach selection guided by surgical goals
How it differs from laparoscopy
- 3D visualization in many systems
- Wristed instruments can improve maneuverability
- Ergonomics may help for long complex cases
- Not required for every minimally invasive case
Important to know
- Not every GI cancer is suitable for robotic approach
- Safety, margins, and oncologic principles come first
- Final plan is individualized after evaluation
If any of the linked pages aren’t live yet, keep the links—publish those pages next to build the full cluster.
Who May Be Considered for a Robotic Approach?
“Robotic” is not a default choice; it is one of the approaches that may be considered after reviewing imaging, diagnosis, and surgical goals. In GI oncology, a minimally invasive (laparoscopic/robotic) plan may be discussed for some patients when oncologic safety and feasibility are met.
Factors that often influence suitability
- Tumor site & stage: localized vs advanced spread
- Imaging findings: relation to major vessels and organs
- Prior surgeries: adhesions or altered anatomy
- Overall fitness: anesthesia risk, nutrition, comorbidities
- Procedure complexity: reconstruction needs, lymph node dissection
Reasons an open approach may be preferred
- Need for extensive multi-organ resection
- Complex vascular involvement
- Dense adhesions from prior major operations
- Intraoperative findings requiring conversion for safety
Conversion to open surgery is a safety decision when needed and does not mean the plan “failed.”
Practical tip: Bring all prior reports—biopsy (if done), PET/CT or contrast CT, MRI (if done), endoscopy/colonoscopy reports, and prior operation notes. These help determine the safest surgical pathway.
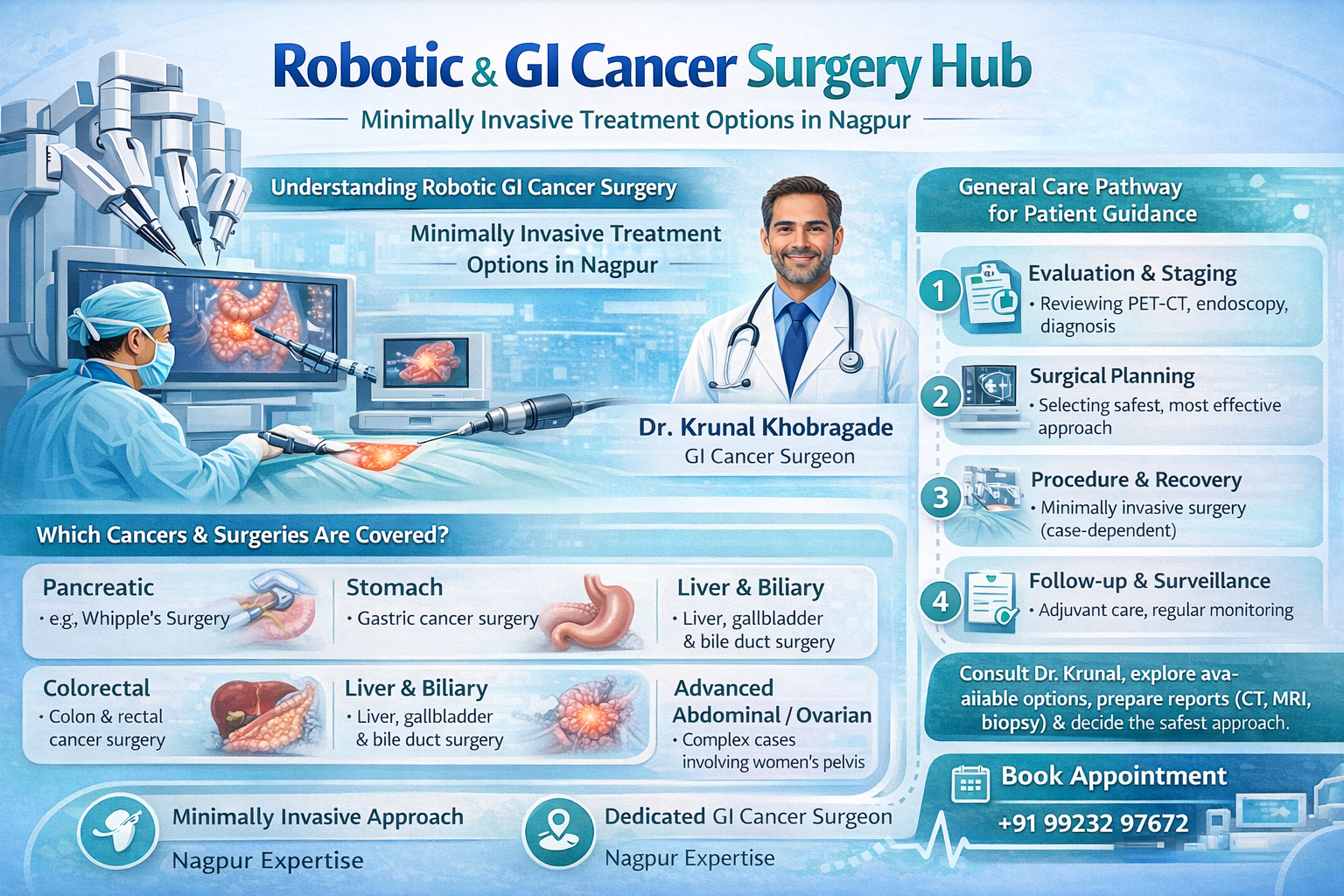
GI Cancers & Surgeries Covered in This Hub
“GI cancers” typically refers to cancers of the digestive system and nearby organs. Below is a navigation-style overview to help you jump to the right procedure page.
Pancreas
Stomach & Upper GI
Liver & Biliary
Peritoneal / Advanced Abdominal
Women’s cancers (GI-linked care)
Typical Care Pathway for GI Cancer Surgery
1) Evaluation & staging
- Review of symptoms, history, and prior treatments
- Imaging review (contrast CT / PET-CT / MRI as applicable)
- Endoscopy/colonoscopy and biopsy reports (if performed)
- Staging to plan curative-intent vs disease-control approaches
2) Surgical planning
- Decision on approach: open vs laparoscopic vs robotic (case-dependent)
- Planning of lymph node dissection and reconstruction needs
- Assessment of nutrition and fitness for surgery
- Discussion of risks, expected hospital course, and follow-up
3) Surgery & immediate recovery
- Anesthesia + procedure performed as planned, with safety-first adjustments if required
- Pain control plan and early mobilization strategies
- Monitoring, drains (if needed), diet progression as advised
4) Pathology, adjuvant planning & surveillance
- Final pathology (margins, lymph nodes, tumor type)
- Coordination with oncology team for chemo/radiation where indicated
- Follow-ups for recovery, nutrition, and long-term monitoring
Whipple’s surgery is a specialized operation for select pancreatic/ampullary/duodenal region tumors and related conditions. If your scans mention “head of pancreas,” “periampullary,” or “distal bile duct,” start with the dedicated page: Whipple’s Surgery in Nagpur.
Recovery, Diet & Follow-up (General Guidance)
Recovery varies by procedure complexity, baseline fitness, and whether reconstruction was needed. Your care team will provide a personalized plan. Below are common themes patients ask about.
Hospital stay
- Monitoring for pain control and early mobility
- Breathing exercises and physiotherapy guidance
- Diet progression based on bowel function and procedure
Diet & nutrition
- Small frequent meals may be advised post major GI surgeries
- Protein and hydration goals as directed
- Supplements/enzyme support only if prescribed
Follow-ups
- Wound review and medication adjustments
- Pathology discussion & next-step planning
- Long-term surveillance schedule as advised
When to seek urgent help: fever, worsening abdominal pain, persistent vomiting, chest pain, shortness of breath, bleeding, or any sudden concerning symptom—contact your treating team or emergency services.
Related Pages
Also Read
Know more
If these pages don’t exist yet, publish them next—these improve navigation and topical authority.
FAQs: Robotic & GI Cancer Surgery
These are common, patient-style questions. Exact eligibility and approach are decided after imaging review and clinical evaluation.
GI cancers typically include cancers of the digestive tract and nearby organs—such as esophagus, stomach, pancreas, liver, gallbladder, small intestine, colon, and rectum. Some advanced abdominal cancers that involve the peritoneum may also be managed within GI oncology pathways.
Not necessarily. The best approach is the one that safely achieves oncologic goals (complete tumor removal where possible, adequate margins, and appropriate lymph node dissection) based on your diagnosis and anatomy. Robotic surgery may be considered for selected cases, but open surgery may be preferred in others.
Eligibility is decided by the treating surgical team after reviewing imaging (CT/PET/MRI as applicable), pathology/biopsy results (if available), your medical fitness, and procedure complexity. The final decision is individualized and may change based on intraoperative findings.
Whipple’s surgery (pancreaticoduodenectomy) is a complex operation commonly discussed for select tumors around the head of the pancreas, periampullary region, and distal bile duct. If your reports mention these areas, review the dedicated page here: Whipple’s Surgery in Nagpur.
Robotic or laparoscopic approaches may be discussed for some colorectal cases depending on tumor location, stage, body habitus, prior surgeries, and the need for complex pelvic dissection. Your surgeon will recommend the most appropriate approach after evaluation.
HIPEC (Hyperthermic Intraperitoneal Chemotherapy) is a specialized treatment used in selected cases of peritoneal involvement from certain cancers. It is often discussed along with cytoreductive surgery (CRS) where visible disease in the abdomen is surgically addressed first. Learn more: Cytoreductive Surgery & HIPEC in Nagpur.
Bring any available imaging disks/reports (contrast CT/PET-CT/MRI), biopsy/pathology reports, endoscopy/colonoscopy reports, blood tests, and records of prior surgeries or treatments. If you have a discharge summary or chemotherapy plan, bring those as well.
Recovery duration varies based on the exact surgery, your baseline health, and whether reconstruction or multi-organ work was needed. Your surgeon will outline expected hospital stay, diet progression, activity guidance, and follow-up timelines based on your plan.
Need guidance for the right next step?
If you have a diagnosis related to pancreas, stomach, colon/rectum, liver, gallbladder, or peritoneal disease, this hub can help you navigate the correct procedure page and prepare for consultation.
